*Free registration is required to use the toolkits provided within HIPxChange. This information is required by our funders and is used to determine the impact of the materials posted on the website.
Background
Interhospital transfers, the movement of patients between acute care facilities, play an increasingly critical role in the United States healthcare system. Although interhospital transfers are necessary, transferred patients experience more morbidity and mortality than directly admitted patients, even after adjusting for severity of illness. Effective and efficient communication between healthcare providers is crucial during interhospital transfers to promote ideal resource allocation as well as optimal patient outcomes and continuity of care. The process of transferring a patient from one hospital to another involves a complex exchange of information and collaboration between providers to decide the best plan of action. Despite best efforts, communication breakdowns and misunderstandings can occur, potentially contributing to delayed and suboptimal patient care. There is preliminary evidence demonstrating that improved communication prior to interhospital transfers may lead to better patient outcomes, including preventing up to 70% of adverse events among transferred critically ill patients.
Transfer centers are centralized departments within hospitals that coordinate the care of transferred patients and the communication between providers at referring and accepting hospitals. The communication between the referring provider, the accepting provider, and the transfer center staff typically follows the sequence depicted in the Figure. Although not all transfer centers are staffed by nurses, we will refer to transfer center staff as transfer center nurses consistent with the terminology utilized by the national Transfer Center Nursing Practice Group, a grassroots organization of transfer center staff, nurses, managers, and medical directors. First, a referring provider requests a transfer through the transfer center nurse. The transfer center nurse collects initial information from the referring provider, such as the diagnosis, and pages the specialty-appropriate on-call accepting provider. Second, the transfer center nurse talks with the accepting provider, summarizing what they heard from the referring provider. Third, the transfer center nurse connects the accepting provider and referring provider so they can discuss the patient and reach a decision about whether to transfer. After a decision is made, the transfer center nurse may also coordinate logistics of the transfer (e.g., securing transportation, bed assignments, and insurance approval, if applicable).
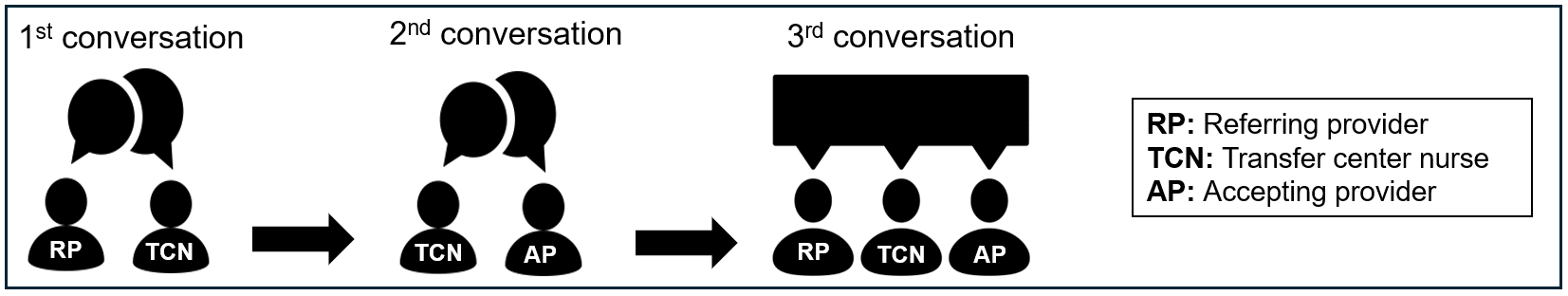
Our research has documented that transfer center nurses face multiple challenges when facilitating conversations about interhospital transfers. During the first conversation (with the referring provider), transfer center nurses face challenges because referring providers, at times, are unfamiliar with the transfer center nurse role, lack awareness of the specialty services at accepting hospitals, and provide incomplete information about the patient. These challenges make it harder for transfer center nurses to get the information they need to accurately and swiftly triage the call to the correct accepting provider. During their second conversation (with the accepting provider), transfer center nurses face challenges because accepting providers have differing preferences regarding the amount of information they desire before connecting with the referring provider; this creates uncertainty for transfer center nurses about how much information to convey to the accepting provider. Accepting providers also, at times, lack awareness of referring hospital capabilities, a critical piece of information in transfer decision-making.
This Transfer Call Toolkit offers tools to help transfer center nurses facilitate calls about transfers and ensure that the information exchange is clear, complete, consistent, and efficient. It also provides resources to facilitate training transfer center nurses on the tools and to communicate to providers and leadership at referring and accepting hospitals that the tools will be used. Streamlining the communication regarding transferred patients may help minimize transfer delays and optimize patient outcomes.
We have also developed tools to support accepting providers in their conversations with referring providers during the third conversation of the transfer call. The Supporting Interhospital Transfer Decisions (SITe) Toolkit can be found here: https://www.hipxchange.org/toolkit/SITeToolkit
Who should use this toolkit?
The Transfer Call Toolkit is intended for anyone who is involved in communication about interhospital transfers, including but not limited to hospital leaders; transfer center managers and directors, nurses, and staff; and referring and accepting providers. The toolkit includes the tools developed; resources for education and training when incorporating the tools into transfer calls; and resources to raise awareness that the tools are being used. Thus, some information contained in the toolkit may not be applicable to all parties listed.
What does the toolkit contain?
| Transfer Call Tools | |
|---|---|
 |
Content checklists
|
 |
Conversation scripts
|
 |
Referring hospital resources template
|
| Resources to promote utilization of and awareness about the tools | |
 |
Resources for training transfer center nurses on and educating accepting providers about the tools
|
 |
Resources for accepting hospitals to communicate their utilization of the tools to referring facilities and providers
|
How can these tools and resources be used?
This toolkit offers suggested methods and resources to help accepting hospitals and transfer centers put the tools to use and raise awareness about the tools. A copy of each tool and resource is available as a Microsoft file so hospitals can adapt the materials for their own preferences and circumstances. Accepting hospitals and transfer centers can use these tools and resources to:
1. Train transfer center nurses on the tools
- Incorporate checklists, scripts, and the referring hospital resources template into the transfer center’s standard operating procedures, internal documents, websites, and electronic medical record documentation
- Hold trainings for existing transfer center nurses
- Incorporate tool(s) into onboarding of new transfer center nurses
2. Educate accepting providers about the tools
- Inform current accepting providers that the tools will be utilized in transfer calls
- Include information about the tools in onboardings of new providers
3. Communicate about utilization of the tools with referring facilities and providers
- Update external-facing information sources, such as transfer center websites and call center recordings
- Communicate with referring hospitals and providers about use of the new tools
Development of this toolkit
The Transfer Call Toolkit was designed as part of a larger study aimed at understanding and addressing communication challenges experienced by providers and transfer center nurses during interhospital transfers of emergency general surgery patients. We first interviewed transfer center nurses, accepting providers, and referring providers about their experiences with communication challenges during transfer calls. Information gleaned from these interviews informed the materials presented to a stakeholder group that helped develop this toolkit.
The Emergency General Surgery Transfer Stakeholder Group was composed of two accepting surgeons, two referring surgeons, two referring emergency medicine physicians, and two transfer center nurses. The group engaged in four 90-minute virtual meetings between October 2022 and April 2023. Stakeholders collaborated to design an intervention to address key communication challenges experienced by providers and transfer center nurses during transfer calls about patients with emergency general surgery diagnoses.
To accomplish this, our research team and the Emergency General Surgery Transfer Stakeholder Group completed the following activities:
Meeting 1:
- Introduced stakeholders to their peers and the research team
- Presented previous research on interhospital transfers of emergency general surgery patients
- Discussed communication challenges experienced during emergency general surgery transfer calls
Meeting 2:
- Identified possible interventions to address top communication challenges
- Reached consensus on which interventions to develop further (content lists and scripts)
Meeting 3:
- Discussed details of what information should be included in contents lists and scripts for the first and second conversations of the transfer call
Meeting 4:
- Refined toolkit components
- Discussed toolkit implementation and dissemination strategies
- After incorporating feedback from Meeting 4, the research team disseminated the toolkit to the stakeholders for final review and edits.
Acknowledgements
The research team is grateful to the members of the Emergency General Surgery Transfer Stakeholder Group for their enthusiasm and dedication to this project. Stakeholders included:
Referring surgeons: Jill Ties, MD (St. Croix Health); Neel Karne, MD, MBA (Beloit Health System)
Referring emergency medicine physicians: David Hindle, MD (University of Wisconsin-Madison); Christopher Stahmer, MD (MEP Health)
Accepting surgeons: Thomas Carver, MD (Medical College of Wisconsin); Hee Soo Jung, MD (University of Wisconsin-Madison)
Transfer center nurses: Nikki Karlen, BSN, RN (UW Health-Meriter Access Center); David Anderson, BSN, RN (UW Health-Meriter Access Center)
The research team would also like to thank the following individuals who have provided valuable insights, support, and effort to the research team and our pursuit of this research:
- Esra Alagoz, PhD
- Natalia Arroyo, MPH
- Sara Fernandes-Taylor, PhD
- Fiona Ljumani, BS
- Jessica Schumacher, PhD
- Gretchen Schwarze, MD, MPP
This development of the toolkit was supported by the Agency for Healthcare Research and Quality (5K08HS025224-05). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
The project described was also supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR002373. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Please send questions, comments, and suggestions to aingraham.md.ms@gmail.com.
Toolkit Citation
Gutierrez-Meza D, Saucke M, Ingraham A. Transfer Call Toolkit. University of Wisconsin – Madison Department of Surgery. Madison, WI; 2024. Available at: http://www.hipxchange.org/toolkit/TransferCallToolkit

 The health services research program of Angela Ingraham, MD, MS, focused on improving care and outcomes of emergency general surgery (EGS) patients, particularly among those who are transferred between acute care facilities. Dr. Ingraham was funded by the Agency for Healthcare Research and Quality through a Career Development Award (5K08HS025224-05) to develop this toolkit. Her National Institute on Aging-funded research (5R03AG078889-02) aimed to standardize communication about transfer decisions by developing an intervention to Support Interhospital Transfer Decisions (SITe) that is specific to the needs of older EGS patients
The health services research program of Angela Ingraham, MD, MS, focused on improving care and outcomes of emergency general surgery (EGS) patients, particularly among those who are transferred between acute care facilities. Dr. Ingraham was funded by the Agency for Healthcare Research and Quality through a Career Development Award (5K08HS025224-05) to develop this toolkit. Her National Institute on Aging-funded research (5R03AG078889-02) aimed to standardize communication about transfer decisions by developing an intervention to Support Interhospital Transfer Decisions (SITe) that is specific to the needs of older EGS patients