*Free registration is required to use the toolkits provided within HIPxChange. This information is required by our funders and is used to determine the impact of the materials posted on the website.
Background
Interhospital transfers for emergency general surgery (EGS) conditions have increased in recent years in the United States (US). Older patients with EGS diagnoses are more likely to be transferred between hospitals and experience worse outcomes than younger patients. A contributing factor to these worse outcomes is that care coordination suffers during interhospital transfers. Provider communication is particularly critical to decisions about transfers of older adults due to circumstances that are unique to their care. Comorbid conditions and acute illness can limit older adults’ cognitive capacity to provide their health history and fully participate in medical decision-making, including transfer decisions. Interhospital transfers also fragment care and separate older adults from their regular healthcare providers and, sometimes, their family support and surrogate decision makers, who often advocate for their needs and medical decision-making.
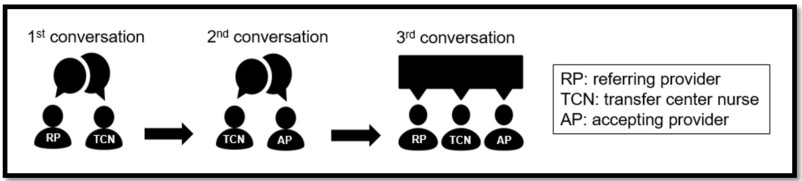
Most (84%) US tertiary centers require a 3-way conversation between referring providers, accepting surgeons, and transfer center nurses before any transfer. Transfer centers are centralized departments within hospitals that coordinate the care of transferred patients and the communication between providers at referring and accepting hospitals. This communication typically follows the sequence depicted in the Figure. First, a referring provider requests a transfer through the transfer center nurse. The transfer center nurse collects initial information from the referring provider, such as the diagnosis, and pages the specialty-appropriate on-call accepting provider. Second, the transfer center nurse talks with the accepting provider, summarizing what they heard from the referring provider. Third, the transfer center nurse connects the accepting provider and referring provider so they can discuss the patient and reach a decision about whether to transfer. After a decision is made, the transfer center nurse may also coordinate logistics of the transfer (e.g., securing transportation, bed assignments, and insurance approval, if applicable).
Our interviews of transfer center nurses and referring and accepting providers have demonstrated that conversations discussing decisions to transfer EGS patients are ineffective, incomplete, and inefficient. Participants outlined a range of interconnected communication challenges including:
- A lack of standardized list of information to share
- Inefficient and incomplete sharing of information between providers
- The reason for transfer not always being clearly communicated
- The accepting surgeon not always being aware of the resources available at referring hospital
- The referring provider not always knowing what the transfer center nurse told the accepting surgeon and how much information should repeated
We have already developed tools to support transfer center nurses in their conversations with providers during the first and second conversations of the transfer call. The Transfer Call Toolkit can be found here: https://www.hipxchange.org/toolkit/TransferCallToolkit
The Supporting Interhospital Transfer Decisions (SITe) Toolkit was specifically designed to assist accepting providers during the third conversation of the transfer call. The tools are a script and checklist to help accepting providers guide the conversation with the referring provider. Accepting providers were selected as the target user because they lead the 3-way conversation and know what information they need to make a decision about transfer. In addition to the tools, the SITe Toolkit contains resources to train accepting providers and to increase awareness of use of the tools among other parties involved in interhospital transfers.
Who should use this toolkit?
The SITe Toolkit was developed to support communication between referring and accepting providers when discussing interhospital transfers. The tools were designed to be used by accepting surgeons when discussing older adults with EGS diagnoses. However, the tools can be easily adapted for other service lines and patient populations, so accepting providers of any kind may benefit from using these tools. The resources to promote utilization of and awareness about the tools are useful for anyone who is directly or indirectly involved in communication about interhospital transfers or in leadership positions at accepting hospitals (e.g., transfer center nurses, managers, and directors and hospital leadership).
What does the toolkit contain?
| SITe Tools | |
|---|---|
  |
3-way conversation script & content checklist
|
| Resources to promote utilization of and awareness about the tool | |
 |
Resources for training accepting providers on the tools
|
 |
Resources to communicate utilization of the tool to providers and transfer center staff
|
How can these tools and resources be used?
The SITe tools are a script and content checklist. The script is intended to help guide the conversation. The content checklist provides accepting providers a list of items to discuss during the conversation between referring and accepting providers. We do not anticipate that accepting providers will check off all items on the content checklist or use the script verbatim. However, reviewing the content checklist and incorporating some scripted language may help to ensure that the accepting provider has the necessary information to make a transfer decision and care for the patient when they arrive.
Individual accepting providers are welcomed and encouraged to familiarize themselves with and use the SITe tools independently. The tools are simple such that with minimal effort providers can become familiar with the tools. To facilitate independent learning, we have provided a recording of the initial training completed by University of Wisconsin accepting surgeons. The training portion of the recording is 20 minutes on normal speed (15 minutes on 1.25x). Toward the end, at about 20 minutes in, we have included the discussion that the providers had after completing their role plays; viewing this is optional but encouraged.
Facilitated group training provides an enhanced experience due to the opportunity to practice using the tools through role-play activities, which necessitates more than one person. We have outlined below the use of the SITe Toolkit in the context of a group training.
This toolkit also offers suggested methods and resources to (1) train accepting providers on the tools and (2) communicate to relevant parties that the tools are being used. The resources can be used together or separately.
Suggested methods to introduce and encourage accepting providers to use the SITe tools
1. Hold trainings for existing accepting providers and incorporate tool(s) into onboarding of new accepting providers. Trainings are intended to last no more than 45 minutes and can utilize these resources:
- PowerPoint slide deck: provides the reasoning for and process used to develop the SITe script and checklist, explanations of the tools, video and audio demonstrations of using the tools, and role play activity instructions
- Training script: a script for the training leader to use with PowerPoint slide deck
- QR code sticker1: a QR code that can be printed on mailing labels to create small stickers that can be placed on the backs of accepting providers’ badges or other locations the providers frequent (e.g., computers in the ORs)
- Role Play Scenario Briefs: hypothetical transfer request scenarios to facilitate role playing to practice using the tools
2. Widely display the QR code (and sticker), script, and checklist. Accepting providers are encouraged to keep the QR code and SITe tools in locations that facilitate use:
- Placing the QR code sticker on their badge
- Saving the tools on their desktop or as a widget on their phone
- Tacking up the tools to personal office bulletin boards
Accepting hospitals can facilitate use by making sure that materials are posted in common areas frequented by accepting providers such as physician lounges, operation rooms, and shared workspaces. The accepting provider flyer provided can be posted in common areas to remind accepting providers to reference the script and checklist during their 3-way transfer calls.
3. Incorporate script and checklist into standard operating procedures and internal documents and drives. Accepting hospitals can include the SITe tools in existing materials and/or save the tools to locations that are referenced and used by accepting providers (e.g., shared drives, intranet sites, onboarding packages, and other documents or locations that are readily accessible to accepting providers during calls).
4. Hold follow-up meetings with accepting providers to encourage use of tools. We suggest having intermittent meetings with accepting providers to discuss how utilization of the script and checklist is going. Some questions to gather feedback include:
- What is going well using the tool(s)?
- What would make using the tool(s) easier?
- Should anything be changed regarding where the tool(s) are displayed or saved?
- Should anything be changed in how we train accepting providers?
Suggested methods for accepting hospitals to communicate their utilization of the SITe tool with their transfer center
Inform transfer center leadership and nurses that the SITe tools will be utilized by accepting providers. We have created SITe flyers and email templates to describe the tools and the changes to anticipate during the conversation between referring and accepting providers. We suggest distributing the script and checklist so that transfer center nurses can review them and ask questions. The flyers can also be posted in common office spaces and work areas. We recommend that the transfer center leadership incorporate information about the tools into onboardings and new hire packets, newsletters, and transfer center meetings.
Give our research team feedback about the tools
Regardless of how the tools are used or adapted, please report back on how you used the SITe toolkit at your own institution https://go.wisc.edu/SITeToolkitFeedback. We are interested to know how using the tools and resources went, what additional refinements or adaptations were made, and what feedback has been provided on the tools and resources.
Also, please share the link for this toolkit freely: https://hipxchange.org/toolkit/SITetoolkit/
Development of this toolkit
The SITe Toolkit was designed as part of a study that aimed to create and pilot-test an intervention to standardize communication about transfer decisions regarding older EGS patients. The SITe Stakeholder Group was composed of two accepting surgeons, two referring surgeons, two referring emergency medicine physicians, two transfer center nurses, and two geriatricians. The group engaged in five 60–90-minute virtual meetings between May 2023 and November 2023. Stakeholders collaborated to design tools to support the conversation between referring and accepting providers.
The research team and the SITe Stakeholder Group completed the following activities. After the stakeholder meetings, the research team incorporated all feedback about training and toolkit resources.
| Meeting 1 | |
|---|---|
|
|
| Meeting 2 | |
|
|
| Meeting 3 | |
|
|
| Meeting 4 | |
|
|
| Meeting 5 | |
|
|
Acknowledgements
The research team is grateful to the members of the SITe Stakeholder Group for their enthusiasm and dedication to this project. Stakeholders included:
- Referring surgeons: Jill Ties, MD (St. Croix Health); Nicholas Kitowski, MD (Krohn Clinic)
- Referring emergency medicine physicians: Kerry Ahrens, MD, MS (Baycare Clinic, University of Wisconsin-Madison); Thanh Tran, MD (Marshfield Medical Center-Beaver Dam)
- Accepting surgeons: Mehreen Kisat, MBBS, MS (University of Wisconsin-Madison); Thomas Carver, MD (Medical College of Wisconsin)
- Transfer center nurses: Nikki Karlen, BSN, RN (UW Health-Meriter Access Center); David Anderson, BSN, RN (UW Health-Meriter Access Center)
- Geriatricians: Elizabeth Chapman, MD (University of Wisconsin-Madison, William S. Middleton Memorial VA Hospital Geriatric Research Education and Clinical Center); Alexis Eastman, MD (University of Wisconsin-Madison)
The research team would also like to thank the following individuals who have provided valuable insights, support, and effort to the research team and our pursuit of this research:
- Esra Alagoz, PhD
- Natalia Arroyo, MPH
- Sara Fernandes-Taylor, PhD
- Jessica Schumacher, PhD
- Nora Jacobson, PhD
This development of the toolkit was supported by the National Institute on Aging through their GEMSSTAR award (1R03AG078889-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health and the National Institute on Aging. Please send questions, comments, and suggestions to aingraham.md.ms@gmail.com
1 The QR code sticker document is meant to be printed on standard address label sheets that contain 30 labels per sheet (3 columns of 10), such as Avery 5160. Once printed, a paper cutter can be used to cut each column in half, resulting in 60 SITe stickers per sheet. We recommend giving accepting surgeons 3-4 stickers each to stick where they see fit.

 The National Institute on Aging-funded research
The National Institute on Aging-funded research